Inside your digestive system lives a vast universe of microorganisms that plays a crucial role in your life. There are roughly 100 trillion bacteria from more than 1,000 different species living in your gut, collectively weighing about 2-5 pounds—about the same as a major organ. This microscopic ecosystem isn’t just helping you digest food; it is also influencing your thoughts, emotions, immune responses, and overall health in ways scientists are only beginning to understand.
The Surprising Gut-Brain Highway
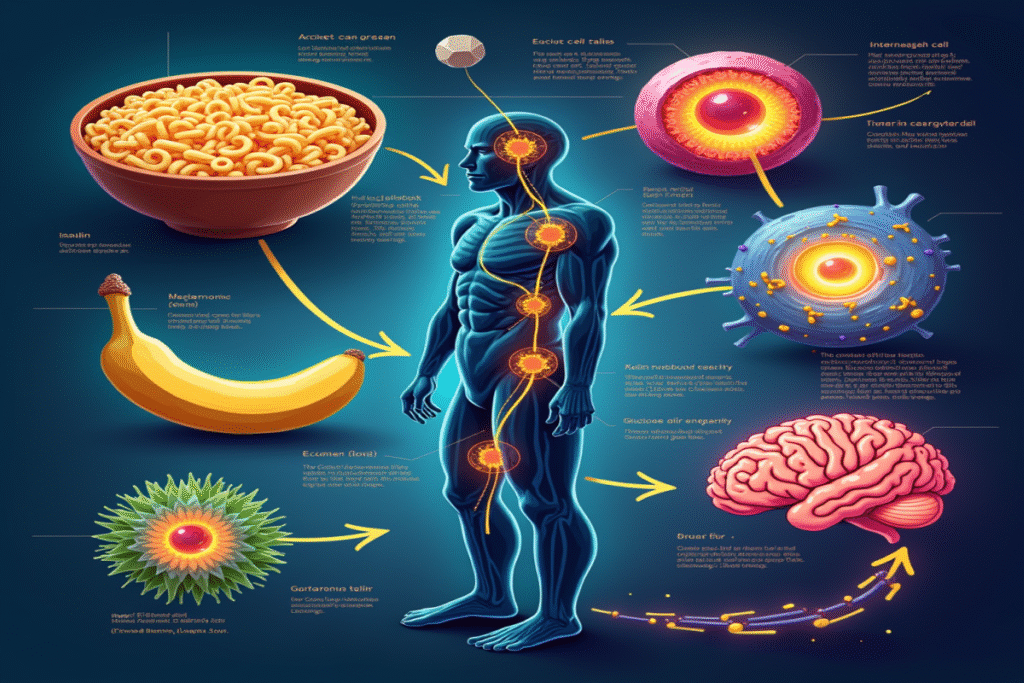
One of the most remarkable discoveries is that your gut and brain are in constant communication via the “gut-brain axis.” This is a two-way communication system involving the vagus nerve (the longest cranial nerve), neurotransmitters, immune pathways, and hormones.
Here’s what’s fascinating: your gut bacteria produce an estimated 95% of your body’s serotonin—the same “happiness molecule” targeted by many antidepressants. This means your intestinal microbes help manufacture chemicals that regulate your mood, anxiety, and happiness.
Your Microscopic Mood Regulators
Research published in prestigious journals like Nature has shown that transferring gut bacteria from people with depression into lab animals can actually cause depressive behaviors in those animals. On the other hand, beneficial bacteria such as Lactobacillus and Bifidobacterium have been found to reduce anxiety and stress levels in studies.
A major 2019 study involving over 1,000 people found that specific patterns of gut bacteria were linked to quality of life and depression. People with higher levels of certain bacteria that produce butyrate (a short-chain fatty acid) reported better mental health and lower depression rates.
The Immune System’s First Trainer
Your gut microbiome acts as a training ground for your immune system. From birth, these bacteria help “educate” your immune cells on what is harmful and what is harmless. It is estimated that 70-80% of your immune tissues are found in your gut, making this relationship vital for your health.
When gut bacterial diversity declines—often due to processed foods, stress, or antibiotics—the immune system can become confused, which may lead to:
- Autoimmune conditions where the body attacks itself
- Chronic inflammation linked to heart disease, diabetes, and cancer
- Increased risk of infections
- Allergic responses to harmless substances
Beyond Digestion: Whole-Body Influence
The influence of the microbiome goes far beyond digestion, mood, and immunity. These tiny inhabitants also affect:
Metabolism and Weight
Identical twins with different gut bacteria can have different abilities to extract calories from the same foods. Some bacteria help absorb more energy, which may lead to weight gain, while others support leanness. One study found that transferring gut bacteria from obese mice to lean mice made the lean mice gain significant weight—even without changing their diet.
Heart Health
Certain gut bacteria break down nutrients in red meat and eggs to produce TMAO (trimethylamine N-oxide), a compound strongly linked to a higher risk of heart disease. Other bacteria help regulate cholesterol and blood pressure.
Brain Development and Aging
The gut microbiome affects brain development in early life and may help protect against cognitive decline as we age. Some studies suggest conditions like Alzheimer’s and Parkinson’s disease may be linked to changes in gut bacteria composition and function.
Nurturing Your Microbial Garden
The good news is that, unlike your DNA, you can shape your microbiome through your daily choices:
Dietary Diversity
Different plant foods provide different fibers and polyphenols that feed varying beneficial bacteria. People who eat more than 30 types of plant foods per week have significantly greater bacterial diversity than those who eat fewer than 10 kinds. Fermented foods like yogurt, kimchi, and sauerkraut also introduce helpful live bacteria.
Movement Matters
Regular exercise increases microbial diversity and boosts the production of beneficial short-chain fatty acids, which reduce inflammation and strengthen the gut barrier.
Stress Management
Chronic stress can quickly change the balance of bacteria in your gut. Practices such as meditation, getting enough sleep, and maintaining social connections all support gut health and resilience.
The Frontier of Personalized Medicine
We are entering a time when microbiome analysis may guide personalized health strategies. Scientists are developing targeted probiotics for conditions like anxiety and obesity, tailored to an individual’s bacterial profile. Some research centers are even working on “psychobiotics”—specific bacterial strains designed to improve mental health.
What’s truly remarkable is how this invisible ecosystem connects us with our environment. Everything from the food we eat to the places we spend time in and the people we meet shapes our microbial companions, who in turn help determine our physical and mental wellbeing.
The next time you get a gut feeling, remember—your microscopic residents are in constant communication with your brain, immune system, and every other part of your body. It’s a beautiful biological symphony that science is only beginning to unravel.